Baby boomers are finding the spirit is often willing, but knees—not so much. Sore and stiff joints seem to arrive just when you line up for your $10 Senior Pass at the U.S. National Parks.
First, know there are two main types of arthritis:
Rheumatoid arthritis (RA) is immunity gone rogue, an autoimmune disorder causing inflammation of joints and other musculoskeletal areas which leads to disability and widespread organ and systemic damage. RA can strike at any age.
Osteoarthritis (OA) , however, sees cartilage on bones in joints erode, losing a vital cushion for knees, hands, hips and spine—the junctures most often debilitated. Time is the big toll-taker here as well as a cluster of other risk factors: gender (female), obesity, injuries, occupation, genetics, bone deformities and other diseases such as diabetes. OA is the most common form of arthritis which affects many millions of people worldwide.
Answers for arthritis
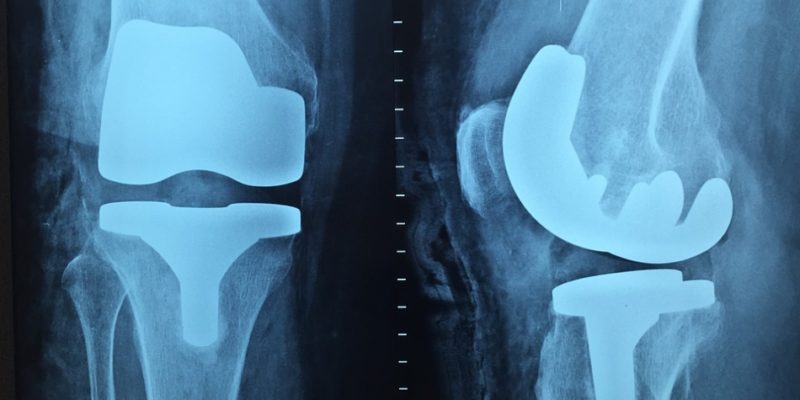
The remedies are many, which means unfortunately, that there’s no one perfect therapy. Pain pills, physical therapy, surgery, and steroids are a few of the common mainstream therapies. Fish oils, botanicals and acupuncture are a smattering of alternative fixes.
Only recently has research pointed to the microbiome.
In RA, a growing body of evidence suggests that aberrations in microbiome may trigger the disease.
In one study, when compared to 30 healthy subjects, a 32 patient cohort with RA displayed intestinal flora changes: reduced lactobacteria and increases of enterococci, clostridia and colibacteria. Animal models also link dysbiosis and inflammatory arthritis, according to a 2014 review.
Similar gut bacteria mapping in patients diagnosed with OA is limited. However, fecal analysis showed elevated counts of species from the genus Enterococcus, Streptococcus, Staphylococcus, Eubacterium, Lactobacillus, Bifidobacterium and Clostridium. Prevotella were seen in 5% of the patients tested.
According to a recent review of OA animal models, a rat model suggests that probiotic Lactobacillus casei could relieve pain, inflammatory responses as well as cartilage degradation.
Researchers also note that people with arthritis often have gut disturbances too. Gastrointestinal disorders including reflux, nausea, abdominal bloating and pain, flatulence, constipation and diarrhea were reported by 18%–39% of study participants.
One line of thinking suggests the following link:
- Altered microbiota irritate the lining of the intestines.
- The intestinal wall becomes “leaky” or more permeable.
- Bacteria cross into the blood.
- Inflammation follows
A healthier group of colonies in the gut may strengthen the wall.
Probiotics or their metabolites could interact with immune cells (antigen presenting cells and T cells) and re-balance pro-inflammatory and anti-inflammatory immune responses.
According to a recent review of OA animal models, probiotic Lactobacillus casei may relieve pain, inflammatory responses as well as cartilage degradation.
Practical advice for those with arthritic pain and immobility:
- Get your microbes in order. Always best are fermented foods: add yogurt to your regimen, daily if possible. Experiment with kefir, kombucha, kimchi, and foods you may shy away from. Kombucha, for example, is a sparkly clean beverage without the thickness of dairy products and supplies different good bacteria.
- Probiotic supplements are advised and until we know more specifics go for a multi-strain, once or twice a day.
- And lastly: Eat loads of prebiotics- fruits and vegetables- to feed the colonies of microbes. Western diets are razing the food supply our microbes need for healthy growth.
Using prebiotics and probiotics to alleviate arthritis may loosen up your joints; they certainly won’t hurt.